|
For the last few weeks I’ve been posting about a six week course I’ve been taking called Psychology and Mental Health: Beyond Nature and Nurture. Today is the penultimate week and we have been consolidating the last four weeks learning and identifying how these psychological insights can help us and our clients maintain mental health and well-being. We looked at a recent UK Government report into well-being and considered how we might be able to incorporate its findings into our professional practice. The report was drafted by a team at the new economics foundation (NEF) and presented evidence for things individuals could do themselves to achieve greater well-being. They concluded that people should follow a well-being equivalent of the ‘five fruit and vegetables a day’ rule. You can view the full report here. In summary, they recommended the following:  Keep active When people are physically active they tend to have better mental health. Simple things like going for a walk, mowing the lawn, washing the car are just as effective as going to the gym or running.  Maintain relationships There are things that people can do every day to maintain their connectivity with other people, and to maintain their relationships. Phone a relative/friend, send a postcard, write a letter, or even use social media.  Learn It doesn't have to be formal learning at a university or college, it could be as simple as reading a newspaper/book, doing a crossword or going to the library. Things that keep the brain active and engaged are good for our mental health.  Give Research has shown that people who give – time, money and/or energy – tend to have better mental health than those who don’t.  Be mindful There's a growing body of evidence that an approach called mindfulness is good for our mental health. And that means that every day we can make sure, we can bear in mind, to be aware of the things that we're looking at, the things that we're smelling, the things that we're seeing, our own thoughts, and the functioning of our own bodies, to be aware of and to be engaged with the world rather than just simply passively moving through it. We also looked at a selection of resources available to help maintain mental health and well-being. I thought you might also be interested as they can be used to inform personal or professional strategies. Here they are... Catch It, Check It, Change It The University of Liverpool has recently developed a smartphone app for iPhone and Android. Designed to introduce key ideas from cognitive behavioural therapy (CBT), the app allows users to keep a record of their moods, therefore allowing them to reflect on what affects their feelings. It is hoped that this, in turn, will help them to control their moods. It is not proposed that the app could or would ever replace direct therapy; rather the purpose is to provide an understanding of CBT; helping people to gain a little more insight into, and control over, their emotions. Activity Scheduling Activity is an excellent anti-depressant. But when people are depressed, they often find it difficult to motivate themselves to become active. So clinical psychologists often give their clients simple diaries to keep track of their activity. The BBC’s Activity Scheduling guide is a fantastic resource that you could use yourself or incorporate into your practice with clients. Graded Exposure Anxiety is a common problem which can be reduced through a well-tested therapeutic approach called graded exposure. The basic aim is to help people gradually build up their confidence in addressing a problem that causes them anxiety; step by step. You might find this graded exposure activity sheet helpful. Structured Problem Solving Research has found that rumination can be a key problem in maintaining mental health. However, it has also been found to be a protective factor for people if they had well-developed skills in ‘adaptive coping’. One approach to helping people develop these kinds of skills is called ‘structured problem solving’. This really means breaking down problems into their constituent components and generating possible solutions for each element. Again, the BBC has a simple worksheet available which you might like. Next week will be the last session and I've been told we will be looking at how we can use what we have learned so far to design and commission better mental health and well-being services. If this is something you'd be interested in reading about please follow me on facebook so that you don't miss it. Have a great week!
0 Comments
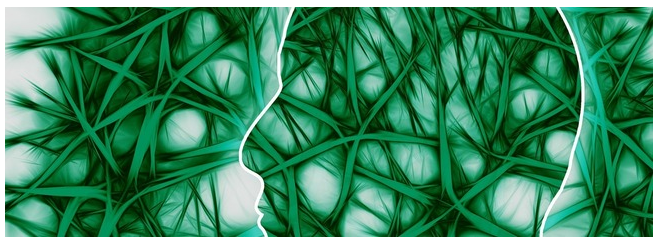
For the last three weeks I've been posting about a course I've been taking called Psychology and Mental Health: Beyond Nature and Nurture. This week we focused on the role of psychological mechanisms in the development of mental health problems and the maintenance of well-being. The sources we were presented with suggest that a psychological perspective adds a vital additional element to the ‘nature-nurture’ debate, because it is through these psychological mechanisms that we interpret and respond to the world.  Our course leader Peter Kinderman, Professor of Clinical Psychology at the University of Liverpool, argues that our mental health is essentially a psychological issue, and that biological, social, and circumstantial factors affect our mental health and well-being by disrupting or disturbing psychological processes. The way in which we make sense of the world, the way in which we understand ourselves, who we are as people, the way we make sense of other people, the way that we react socially, how we think about the future, and how we think about the world in general, this sense making, this framework of understanding of the world is fundamentally important in determining our mental health and well-being. To get us started we are provided with a copy of Peter Kinderman’s, A Psychological Model of Mental Disorder. This article discusses the relationship between biological, social, and psychological factors in the causation and treatment of mental disorder. He suggests that a comprehensive psychological model of mental disorder can offer a coherent, theoretically powerful alternative to reductionist biological accounts while also incorporating the results of biological research. We are told that Peter was able to test out some of these ideas in a research study that he conducted with the help of the BBC; testing out the idea of whether a combination of different factors could predict the level of mental health difficulties and well-being that a person was experiencing. They were interested in whether biological factors, which were measured by looking at the experience of mental health problems in a person's family of origin, in their parents and in their siblings, could predict mental health problems, which would then have a variety of psychological and social consequences. Or whether, on the other hand, life events like trauma in early childhood or experiencing a range of negative life events in the last six months would predict people's mental health problems. Or as they hypothesised, whether psychological factors - rumination, where people would go over and over things in their minds, or self blame, where people would blame themselves for the difficulties they were experiencing - would explain more of a person's mental health problems. When they looked at the results, it seemed that social factors were very influential in predicting people's mental health problems, with biological factors playing a part, but a less important part. But importantly, both social and biological factors were mediated by the psychological factors. So, they asserted, rumination and self blame seem to be the gateways towards mental health problems.
You can see the paper itself and also a brief magazine article (Rumination: The danger of dwelling) hosted by the BBC on their website. Peter says that this way of thinking about mental health has some quite profound consequences. If you realise the way in which a person thinks about the world, the way in which a person responds to events in their lives, makes a difference to their mental health, to their well being, to anxiety and depression, it does change the way in which we should approach mental health problems. It brings it back to the idea that how we think about the world matters. Because it changes the way in which we feel and behave. This gives us some different opportunities for how to help people who've got emotional difficulties. But it's also important for people who themselves are suffering, because rather than blaming them for their difficulties, it means that there are things that they can do themselves to get out of the problems that they find themselves in. It gives people a sense of agency and control over their own mental health. Finally we were invited to take part in some of Peter’s current research: Causal and mediating factors in mental health and wellbeing. A follow up study to the research that has formed the basis of this week’s part of the course. At the end of the course we are asked if we believe adding psychological processes to the mix add anything useful to our understanding of the ‘nature-nurture’ debate? Do we think these kinds of factors are important in determining our mental health and well-being? Do we think an understanding of psychological processes mean that we can offer more useful ways of helping people - perhaps through therapy? What do you think? If rumination is posing a difficulty for you or a client there are a couple of things you could try.
For the last two weeks I've been posting about a course I've been taking called Psychology and Mental Health: Beyond Nature and Nurture. So far I've found it really interesting and it has challenged me to reflect on my practice and past cases.
Last week, we discussed the role of biological processes and mechanisms. We were urged to consider how our emotions, thoughts and behaviours are related to neurotransmitter and other biological mechanisms; and to appreciate how this shapes service provisions. This week we were taught about the role of psychological mechanisms in the development of mental health problems and the maintenance of well-being. The material we were presented with highlighted a vital element to the ‘nature-nurture’ debate, asserting that it is through these psychological mechanisms that we interpret and respond to the world. Many psychologists and psychiatrists believe that it's by looking at the nurture side of the equation, by looking at differences between people in terms of the things that happened to them that we can start to explain mental health issues. Our lecturer says that undoubtedly just from the sheer weight of evidence psychosocial events are the more powerful predictor. We heard about Professor John Read, who believes that the best way to explain the origin of mental health problems - and especially differences between people - is by looking at life events and the different experiences we have in our lives. To get things started we are presented with an article from The British Journal of Psychiatry within which Pat Bracken and colleagues set out an argument for a more social psychiatry; arguing that social factors are the most important determinants of our mental health. Here is their 2012 paper if you’d like to have a read yourself. They argue “… that psychiatry is in the midst of a crisis. The various solutions proposed would all involve a strengthening of psychiatry’s identity as essentially ‘applied neuroscience’. Although not discounting the importance of the brain sciences and psychopharmacology, we argue that psychiatry needs to move beyond the dominance of the current, technological paradigm. This would be more in keeping with the evidence about how positive outcomes are achieved and could also serve to foster more meaningful collaboration with the growing service user movement…”. They says that: ”… Although mental health problems undoubtedly have a biological dimension, in their very nature they reach beyond the brain to involve social, cultural and psychological dimensions. These cannot always be grasped through the epistemology of biomedicine. The mental life of humans is discursive in nature. … The evidence base is telling us that we need a radical shift in our understanding of what is at the heart (and perhaps soul) of mental health practice. If we are to operate in an evidence-based manner, and work collaboratively with all sections of the service user movement, we need a psychiatry that is intellectually and ethically adequate to deal with the sort of problems that present to it. As well as the addition of more social science and humanities to the curriculum of our trainees we need to develop a different sensibility towards mental illness itself and a different understanding of our role as doctors…”. Next we looked at a paper recently published in the journal ‘Schizophrenia Bulletin’ by Filippo Varese and colleagues that I found very interesting as a Children’s Social Worker. Filippo and colleagues explored the link between traumatic childhood experiences (poverty, abuse, etc) and later psychotic experiences. We are told that their work was important because many people tend to think that such serious problems as hallucinations and delusional beliefs are quintessentially biological in origin, and this paper suggests an important social dimension. They looked at a wide range of studies that examined the links between life events and later psychosis. Their conclusions were: ”…Evidence suggests that adverse experiences in childhood are associated with psychosis. To examine the association between childhood adversity and trauma (sexual abuse, physical abuse, emotional/psychological abuse, neglect, parental death, and bullying) and psychosis outcome … we included 18 case-control studies… 10 prospective and quasi-prospective studies… and 8 population-based cross-sectional studies... There were significant associations between adversity and psychosis across all research designs …. patients with psychosis were 2.72 times more likely to have been exposed to childhood adversity than controls. The association between childhood adversity and psychosis was also significant ... These findings indicate that childhood adversity is strongly associated with increased risk for psychosis…” We are directed to read a paper by Ben Barr and colleagues which looked at how the recent economic recession impacted on suicide rates - a rather dramatic (and sad) example of how social factors impact on our mental health. They found that between 2008 and 2010, there were 846 more suicides among men than would have been expected based on historical trends, and 155 more suicides among women. Next we look at a paper in ‘The Psychologist’ by John Read which expresses some frustration at how attempts to integrate biological, social and psychological perspectives on mental health problems tend tacitly to assume that the most important elements are biological, with the social and psychological elements somewhat downplayed. Read argues that people pay lip-service to the bio-psychosocial model, but undermine it in practice. He gives the example of a senior colleague who: ”…acknowledged some of the recent research about the role of psychosocial factors influencing schizophrenia. He concluded, however, that ‘the schizophrenia wars were over years ago’. He was referring to the truce established under the banner of the ‘bio-psycho-social’ model, which says that schizophrenia is an interaction between a genetically inherited predisposition and the triggering effect of social stressors…” He concludes: ”…The simple truths are that human misery is largely inflicted by other people and that the solutions are best based on human – rather than chemical or electrical – interventions…”. Reading this article I can’t help but remember the men I worked with at a service for ex-offenders with drug misuse issues. Most had a dual diagnosis, a number of them schizophrenia, and all had experienced some form of trauma in their childhood or youth. Each of them received medication to treat the condition but “human intervention” was patchy. Our lecturer tells us that we know following 20, 30 years of research that there is no specific genetic predisposition to any of the mental health disorders. And we know that the best predictors by far of all of them, whether it's depression, suicidality, psychosis, are all life events. The strongest predictor all by itself is poverty. Not because poverty by itself causes depression, but because it is a predictor of all the other things that are causal. So poverty has been described as the cause of the causes. And those other causes are a whole raft of things - childhood neglect, childhood abuse, loneliness, and problematic parenting, which is usually inter-generational. It's not about bad parents, it's about parents who themselves haven't perhaps had the sort of childhood that predisposed them to good enough parenting. This is why preventative services, family support and intervention are so vital. Parents need to be taught and supported to break this cycle; and so that children can be safeguarded in the care of their family. This week’s session has left me with little doubt that I favour the social model (this probably won’t come as a surprise to you as I am a Social Worker and Sociology graduate). I hope that following today’s general election we see a greater investment in mental health services as promised in so many of the parties manifestos. I also hope that the next government values children’s social care enough to invest in it and address the woefully inadequate funding for preventative / support services in this country. Spending cuts and austerity have most definitely fallen hardest on the most vulnerable. Have a great week and don’t forget to follow me on facebook so you don’t miss next week’s post on psychology and mental health. Last week I posted about a course I started entitled Psychology and Mental Health: Beyond Nature and Nurture. Last week's class provided a general introduction to the subject matter and what we should expect from the course over the next few weeks. I was keen to get started.
This week we discussed the role of biological factors - nature - in the development of mental health problems. We heard from Professor John Quinn, who outlined some ways in which neurotransmitter activity affects our moods, and is itself affected by events. We looked at Eric Kandel's 'new intellectual framework for psychiatry'. Eric Kandel is a Nobel prize winning neuroscientist. In addition to his work on memory, Kandel was the author of a very influential and important paper setting out a robust biological account of psychiatry. He argues that all human behaviour, thought and emotion has its roots in the functioning of the brain. Consequently it is to brain-based, neuroscientific, explanations that we should look to for solutions to mental health problems. Kandel argues, in the abstract of his paper, that: ”…In an attempt to place psychiatric thinking and the training of future psychiatrists more centrally into the context of modern biology, the author outlines the beginnings of a new intellectual framework for psychiatry that derives from current biological thinking about the relationship of mind to brain. The purpose of this framework is twofold. First, it is designed to emphasize that the professional requirements for future psychiatrists will demand a greater knowledge of the structure and functioning of the brain than is currently available in most training programs. Second, it is designed to illustrate that the unique domain which psychiatry occupies within academic medicine, the analysis of the interaction between social and biological determinants of behavior, can best be studied by also having a full understanding of the biological components of behaviour…” Kandel then sets out five principles that he believes should provide the underpinnings of a ‘new intellectual framework for psychiatry’. “This framework can be summarized in five principles that constitute, in simplified form, the current thinking of biologists about the relationship of mind to brain.” These are: “Principle 1. All mental processes, even the most complex psychological processes, derive from operations of the brain. The central tenet of this view is that what we commonly call mind is a range of functions carried out by the brain. The actions of the brain underlie not only relatively simple motor behaviors, such as walking and eating, but all of the complex cognitive actions, conscious and unconscious, that we associate with specifically human behavior, such as thinking, speaking, and creating works of literature, music, and art. As a corollary, behavioral disorders that characterize psychiatric illness are disturbances of brain function, even in those cases where the causes of the disturbances are clearly environmental in origin.” “Principle 2. Genes and their protein products are important determinants of the pattern of interconnections between neurons in the brain and the details of their functioning. Genes, and specifically combinations of genes, therefore exert a significant control over behavior. As a corollary, one component contributing to the development of major mental illnesses is genetic.” “Principle 3. Altered genes do not, by themselves, explain all of the variance of a given major mental illness. Social or developmental factors also contribute very importantly. Just as combinations of genes contribute to behavior, including social behavior, so can behavior and social factors exert actions on the brain by feeding back upon it to modify the expression of genes and thus the function of nerve cells. Learning, including learning that results in dysfunctional behavior, produces alterations in gene expression. Thus all of “nurture” is ultimately expressed as “nature.”” “Principle 4. Alterations in gene expression induced by learning give rise to changes in patterns of neuronal connections. These changes not only contribute to the biological basis of individuality but presumably are responsible for initiating and maintaining abnormalities of behavior that are induced by social contingencies.” “Principle 5. Insofar as psychotherapy or counseling is effective and produces long-term changes in behavior, it presumably does so through learning, by producing changes in gene expression that alter the strength of synaptic connections and structural changes that alter the anatomical pattern of interconnections between nerve cells of the brain. As the resolution of brain imaging increases, it should eventually permit quantitative evaluation of the outcome of psychotherapy.” Kandel does not deny that social events are important, but he maintains that social events have their impact on people by affecting the brain: “Viewed in this way, all sociology must to some degree be sociobiology; social processes must, at some level, reflect biological functions. … Nevertheless, it is important to appreciate that there are critical biological underpinnings to all social actions.” Not all psychologists and not all psychiatrists agree with his conclusions, but the paper was definitely worth reading. Next we looked at Nick Craddock and colleagues' 'wake up call for British psychiatry'. Nick Craddock and colleagues drew up a manifesto for the future of psychiatry based at least in part on a biological model of mental health. This 2008 paper was entitled a “Wake-up call for British psychiatry”, and was written by a group of influential and senior psychiatrists. It sets out how a biological model of mental health - the idea that our mental health is determined by our biology - can influence how we design services. Nick and colleagues, in the summary to their paper, argue that: “The recent drive within the UK National Health Service to improve psychosocial care for people with mental illness is both understandable and welcome: evidence-based psychological and social interventions are extremely important in managing psychiatric illness. Nevertheless, the accompanying downgrading of medical aspects of care has resulted in services that often are better suited to offering non-specific psychosocial support, rather than thorough, broad-based diagnostic assessment leading to specific treatments to optimise well-being and functioning. In part, these changes have been politically driven, but they could not have occurred without the collusion, or at least the acquiescence, of psychiatrists. This creeping devaluation of medicine disadvantages patients and is very damaging to both the standing and the understanding of psychiatry in the minds of the public, fellow professionals and the medical students who will be responsible for the specialty’s future. On the 200th birthday of psychiatry, it is fitting to reconsider the specialty’s core values and renew efforts to use psychiatric skills for the maximum benefit of patients”. They begin by arguing that: “… British psychiatry faces an identity crisis. A major contributory factor has been the recent trend to downgrade the importance of the core aspects of medical care”. They argue that this has led to problems: “… In many instances, this has resulted in services that are better suited to delivering nonspecific, psychosocial support rather than a process of thorough, broad-based diagnostic assessment with formulation of aetiology, diagnosis and prognosis followed by specific treatments aimed at recovery with maintenance of functioning…”. and state that: “…Our contention is that this creeping devaluation of medicine is damaging our ability to deliver excellent psychiatric care. It is imperative that we specify clearly the key role of psychiatrists in the management of people with mental illnesses…” Later on, they suggest that: “…In order to follow clinical guidance (such as that provided by the National Institute for Health and Clinical Excellence (NICE)) to develop excellent ‘mental health’ care (for those with mental illness), it is important to recognise that a biomedical component, with access to appropriate facilities and appropriate service pathways, is usually crucial…”. For Nick and colleagues, this is an optimistic vision: “…Major advances in molecular biology and neuroscience over recent years have provided psychiatry with powerful tools that help to delineate the biological systems involved in psychopathology and impairments suffered by patients. We can be optimistic that over the coming years these advances will facilitate the development of diagnostic approaches with improved biological validity and enhanced clinical utility in terms of predicting treatment response. We can expect that completely novel treatments will be developed based on detailed understanding of pathogenesis…”. … “…Psychological and social interventions will, of course, continue to be crucially important in managing psychiatric illness (as they are also in non-psychiatric disorders). However, in addition, patients have the right to expect that biological factors are fully considered and, where appropriate, evidence-based interventions delivered…”. Thirdly, we looked at 'Chemical imbalances'. One powerful idea in the area of mental health is the suggestion that mental health problems result from ‘chemical imbalances’ and that the psychiatric drugs that are commonly prescribed help people because they ‘correct’ these ‘imbalances’. In fact, if you search online for information about mental health problems that is sponsored by pharmaceutical companies, this idea is very common. Dr Joanna Moncrieff is a psychiatrist who has criticised this approach. In essence, her argument is that psychiatric medication has well-recognised effects on the brain, which affect our moods, behaviours and even thoughts, and which can - sometimes - be helpful for people in great distress. But Jo does not support the idea that these drugs are correcting chemical imbalances; and she describes this as the ‘myth of the chemical cure’. Jo advocates that we adopt what she describes as the ‘drug-based’ model of the action of psychiatric medication, rejecting the ‘disease-based’ approach. This does not mean that she believes that the medication is ineffective. She recognises that the medication has a clear effect on our neurotransmitters, and therefore on our emotions and behaviour. But Jo does not believe that this necessarily means that the medication is correcting an underlying abnormality. Finally we concluded with a brief critique of this weeks’ discussions. We are taught that the science and the logical arguments are both strong: we know that the functioning of our brains lies beneath all our behaviours, thoughts and emotions, and so biological approaches cannot be dismissed. And yet, many psychologists and social psychologists think that biological approaches alone cannot fully explain our experience of mental health problems. Next week, we will be looking at social perspectives on mental health. We are challenged, over the course as a whole, to consider how these different approaches can be integrated and to consider the strengths and weaknesses of the biological component of the ‘biopsychosocial model’. I’ll see you again next week… |
AuthorI'm a Qualified Children's Social Worker with a passion for safeguarding and family support in the UK. Archives
August 2016
Categories
All
|