|
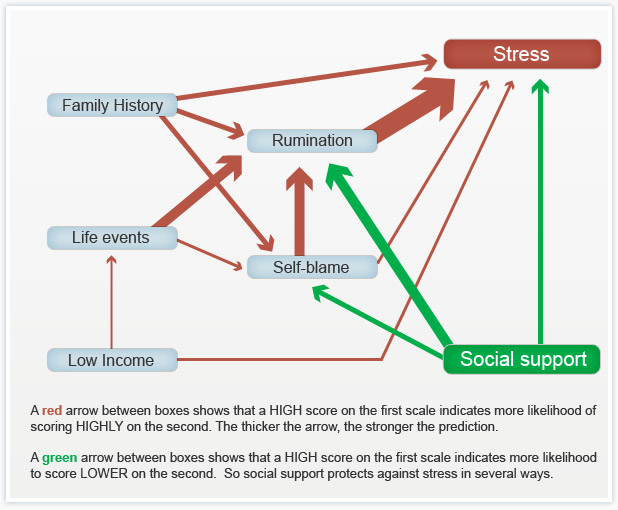
For the last three weeks I've been posting about a course I've been taking called Psychology and Mental Health: Beyond Nature and Nurture. This week we focused on the role of psychological mechanisms in the development of mental health problems and the maintenance of well-being. The sources we were presented with suggest that a psychological perspective adds a vital additional element to the ‘nature-nurture’ debate, because it is through these psychological mechanisms that we interpret and respond to the world.  Our course leader Peter Kinderman, Professor of Clinical Psychology at the University of Liverpool, argues that our mental health is essentially a psychological issue, and that biological, social, and circumstantial factors affect our mental health and well-being by disrupting or disturbing psychological processes. The way in which we make sense of the world, the way in which we understand ourselves, who we are as people, the way we make sense of other people, the way that we react socially, how we think about the future, and how we think about the world in general, this sense making, this framework of understanding of the world is fundamentally important in determining our mental health and well-being. To get us started we are provided with a copy of Peter Kinderman’s, A Psychological Model of Mental Disorder. This article discusses the relationship between biological, social, and psychological factors in the causation and treatment of mental disorder. He suggests that a comprehensive psychological model of mental disorder can offer a coherent, theoretically powerful alternative to reductionist biological accounts while also incorporating the results of biological research. We are told that Peter was able to test out some of these ideas in a research study that he conducted with the help of the BBC; testing out the idea of whether a combination of different factors could predict the level of mental health difficulties and well-being that a person was experiencing. They were interested in whether biological factors, which were measured by looking at the experience of mental health problems in a person's family of origin, in their parents and in their siblings, could predict mental health problems, which would then have a variety of psychological and social consequences. Or whether, on the other hand, life events like trauma in early childhood or experiencing a range of negative life events in the last six months would predict people's mental health problems. Or as they hypothesised, whether psychological factors - rumination, where people would go over and over things in their minds, or self blame, where people would blame themselves for the difficulties they were experiencing - would explain more of a person's mental health problems. When they looked at the results, it seemed that social factors were very influential in predicting people's mental health problems, with biological factors playing a part, but a less important part. But importantly, both social and biological factors were mediated by the psychological factors. So, they asserted, rumination and self blame seem to be the gateways towards mental health problems.
You can see the paper itself and also a brief magazine article (Rumination: The danger of dwelling) hosted by the BBC on their website. Peter says that this way of thinking about mental health has some quite profound consequences. If you realise the way in which a person thinks about the world, the way in which a person responds to events in their lives, makes a difference to their mental health, to their well being, to anxiety and depression, it does change the way in which we should approach mental health problems. It brings it back to the idea that how we think about the world matters. Because it changes the way in which we feel and behave. This gives us some different opportunities for how to help people who've got emotional difficulties. But it's also important for people who themselves are suffering, because rather than blaming them for their difficulties, it means that there are things that they can do themselves to get out of the problems that they find themselves in. It gives people a sense of agency and control over their own mental health. Finally we were invited to take part in some of Peter’s current research: Causal and mediating factors in mental health and wellbeing. A follow up study to the research that has formed the basis of this week’s part of the course. At the end of the course we are asked if we believe adding psychological processes to the mix add anything useful to our understanding of the ‘nature-nurture’ debate? Do we think these kinds of factors are important in determining our mental health and well-being? Do we think an understanding of psychological processes mean that we can offer more useful ways of helping people - perhaps through therapy? What do you think? If rumination is posing a difficulty for you or a client there are a couple of things you could try.
0 Comments
Last week I posted about a course I started entitled Psychology and Mental Health: Beyond Nature and Nurture. Last week's class provided a general introduction to the subject matter and what we should expect from the course over the next few weeks. I was keen to get started.
This week we discussed the role of biological factors - nature - in the development of mental health problems. We heard from Professor John Quinn, who outlined some ways in which neurotransmitter activity affects our moods, and is itself affected by events. We looked at Eric Kandel's 'new intellectual framework for psychiatry'. Eric Kandel is a Nobel prize winning neuroscientist. In addition to his work on memory, Kandel was the author of a very influential and important paper setting out a robust biological account of psychiatry. He argues that all human behaviour, thought and emotion has its roots in the functioning of the brain. Consequently it is to brain-based, neuroscientific, explanations that we should look to for solutions to mental health problems. Kandel argues, in the abstract of his paper, that: ”…In an attempt to place psychiatric thinking and the training of future psychiatrists more centrally into the context of modern biology, the author outlines the beginnings of a new intellectual framework for psychiatry that derives from current biological thinking about the relationship of mind to brain. The purpose of this framework is twofold. First, it is designed to emphasize that the professional requirements for future psychiatrists will demand a greater knowledge of the structure and functioning of the brain than is currently available in most training programs. Second, it is designed to illustrate that the unique domain which psychiatry occupies within academic medicine, the analysis of the interaction between social and biological determinants of behavior, can best be studied by also having a full understanding of the biological components of behaviour…” Kandel then sets out five principles that he believes should provide the underpinnings of a ‘new intellectual framework for psychiatry’. “This framework can be summarized in five principles that constitute, in simplified form, the current thinking of biologists about the relationship of mind to brain.” These are: “Principle 1. All mental processes, even the most complex psychological processes, derive from operations of the brain. The central tenet of this view is that what we commonly call mind is a range of functions carried out by the brain. The actions of the brain underlie not only relatively simple motor behaviors, such as walking and eating, but all of the complex cognitive actions, conscious and unconscious, that we associate with specifically human behavior, such as thinking, speaking, and creating works of literature, music, and art. As a corollary, behavioral disorders that characterize psychiatric illness are disturbances of brain function, even in those cases where the causes of the disturbances are clearly environmental in origin.” “Principle 2. Genes and their protein products are important determinants of the pattern of interconnections between neurons in the brain and the details of their functioning. Genes, and specifically combinations of genes, therefore exert a significant control over behavior. As a corollary, one component contributing to the development of major mental illnesses is genetic.” “Principle 3. Altered genes do not, by themselves, explain all of the variance of a given major mental illness. Social or developmental factors also contribute very importantly. Just as combinations of genes contribute to behavior, including social behavior, so can behavior and social factors exert actions on the brain by feeding back upon it to modify the expression of genes and thus the function of nerve cells. Learning, including learning that results in dysfunctional behavior, produces alterations in gene expression. Thus all of “nurture” is ultimately expressed as “nature.”” “Principle 4. Alterations in gene expression induced by learning give rise to changes in patterns of neuronal connections. These changes not only contribute to the biological basis of individuality but presumably are responsible for initiating and maintaining abnormalities of behavior that are induced by social contingencies.” “Principle 5. Insofar as psychotherapy or counseling is effective and produces long-term changes in behavior, it presumably does so through learning, by producing changes in gene expression that alter the strength of synaptic connections and structural changes that alter the anatomical pattern of interconnections between nerve cells of the brain. As the resolution of brain imaging increases, it should eventually permit quantitative evaluation of the outcome of psychotherapy.” Kandel does not deny that social events are important, but he maintains that social events have their impact on people by affecting the brain: “Viewed in this way, all sociology must to some degree be sociobiology; social processes must, at some level, reflect biological functions. … Nevertheless, it is important to appreciate that there are critical biological underpinnings to all social actions.” Not all psychologists and not all psychiatrists agree with his conclusions, but the paper was definitely worth reading. Next we looked at Nick Craddock and colleagues' 'wake up call for British psychiatry'. Nick Craddock and colleagues drew up a manifesto for the future of psychiatry based at least in part on a biological model of mental health. This 2008 paper was entitled a “Wake-up call for British psychiatry”, and was written by a group of influential and senior psychiatrists. It sets out how a biological model of mental health - the idea that our mental health is determined by our biology - can influence how we design services. Nick and colleagues, in the summary to their paper, argue that: “The recent drive within the UK National Health Service to improve psychosocial care for people with mental illness is both understandable and welcome: evidence-based psychological and social interventions are extremely important in managing psychiatric illness. Nevertheless, the accompanying downgrading of medical aspects of care has resulted in services that often are better suited to offering non-specific psychosocial support, rather than thorough, broad-based diagnostic assessment leading to specific treatments to optimise well-being and functioning. In part, these changes have been politically driven, but they could not have occurred without the collusion, or at least the acquiescence, of psychiatrists. This creeping devaluation of medicine disadvantages patients and is very damaging to both the standing and the understanding of psychiatry in the minds of the public, fellow professionals and the medical students who will be responsible for the specialty’s future. On the 200th birthday of psychiatry, it is fitting to reconsider the specialty’s core values and renew efforts to use psychiatric skills for the maximum benefit of patients”. They begin by arguing that: “… British psychiatry faces an identity crisis. A major contributory factor has been the recent trend to downgrade the importance of the core aspects of medical care”. They argue that this has led to problems: “… In many instances, this has resulted in services that are better suited to delivering nonspecific, psychosocial support rather than a process of thorough, broad-based diagnostic assessment with formulation of aetiology, diagnosis and prognosis followed by specific treatments aimed at recovery with maintenance of functioning…”. and state that: “…Our contention is that this creeping devaluation of medicine is damaging our ability to deliver excellent psychiatric care. It is imperative that we specify clearly the key role of psychiatrists in the management of people with mental illnesses…” Later on, they suggest that: “…In order to follow clinical guidance (such as that provided by the National Institute for Health and Clinical Excellence (NICE)) to develop excellent ‘mental health’ care (for those with mental illness), it is important to recognise that a biomedical component, with access to appropriate facilities and appropriate service pathways, is usually crucial…”. For Nick and colleagues, this is an optimistic vision: “…Major advances in molecular biology and neuroscience over recent years have provided psychiatry with powerful tools that help to delineate the biological systems involved in psychopathology and impairments suffered by patients. We can be optimistic that over the coming years these advances will facilitate the development of diagnostic approaches with improved biological validity and enhanced clinical utility in terms of predicting treatment response. We can expect that completely novel treatments will be developed based on detailed understanding of pathogenesis…”. … “…Psychological and social interventions will, of course, continue to be crucially important in managing psychiatric illness (as they are also in non-psychiatric disorders). However, in addition, patients have the right to expect that biological factors are fully considered and, where appropriate, evidence-based interventions delivered…”. Thirdly, we looked at 'Chemical imbalances'. One powerful idea in the area of mental health is the suggestion that mental health problems result from ‘chemical imbalances’ and that the psychiatric drugs that are commonly prescribed help people because they ‘correct’ these ‘imbalances’. In fact, if you search online for information about mental health problems that is sponsored by pharmaceutical companies, this idea is very common. Dr Joanna Moncrieff is a psychiatrist who has criticised this approach. In essence, her argument is that psychiatric medication has well-recognised effects on the brain, which affect our moods, behaviours and even thoughts, and which can - sometimes - be helpful for people in great distress. But Jo does not support the idea that these drugs are correcting chemical imbalances; and she describes this as the ‘myth of the chemical cure’. Jo advocates that we adopt what she describes as the ‘drug-based’ model of the action of psychiatric medication, rejecting the ‘disease-based’ approach. This does not mean that she believes that the medication is ineffective. She recognises that the medication has a clear effect on our neurotransmitters, and therefore on our emotions and behaviour. But Jo does not believe that this necessarily means that the medication is correcting an underlying abnormality. Finally we concluded with a brief critique of this weeks’ discussions. We are taught that the science and the logical arguments are both strong: we know that the functioning of our brains lies beneath all our behaviours, thoughts and emotions, and so biological approaches cannot be dismissed. And yet, many psychologists and social psychologists think that biological approaches alone cannot fully explain our experience of mental health problems. Next week, we will be looking at social perspectives on mental health. We are challenged, over the course as a whole, to consider how these different approaches can be integrated and to consider the strengths and weaknesses of the biological component of the ‘biopsychosocial model’. I’ll see you again next week… |
AuthorI'm a Qualified Children's Social Worker with a passion for safeguarding and family support in the UK. Archives
August 2016
Categories
All
|